Exclusive Expert Interview
Interviewed by: Samaran, Founding Editor
Guest: Dr. Soundariya S — Senior Clinical Dietitian & Researcher | Wellness & Nutrition Influencer

—
In this exclusive conversation, Founding Editor Samaran speaks with Dr. Soundariya S, a leading clinical dietitian and prominent voice in evidence-based nutrition communication. The discussion delves into precision nutrition, emerging metabolic science, gut microbiome myths, and the nutritional challenges shaping urban India.
—
1. The most consequential development is precision nutrition driven by individual post-prandial glycemic phenotypes and multi-omic data (microbiome + clinical + lifestyle) combined with AI-driven prediction models — this lets us move from population-level advice to tailored meal and timing prescriptions (e.g., CGM-guided food choices and microbiome-informed adjustments), which has the potential to markedly improve glycaemic control and weight outcomes.
In clinical practice, we may shift from one-size-fits-all dietary guidelines to data-driven, individualized nutrition prescriptions — using CGM, metabolomics or gut microbiota data to guide meal composition, timing, and macronutrient distribution. This could refine management of metabolic disorders (pre-diabetes, T2DM, obesity), optimize glycemic control, and reduce complications.
Dr. Soundariya S:
Precision nutrition is undoubtedly the next major leap in metabolic health and dietetics. The integration of post-prandial glycemic phenotypes with multi-omic datasets—microbiome profiles, clinical biomarkers, lifestyle metrics—allows us to personalise dietary plans in a way never before possible. With AI-enabled prediction models, we are moving from broad dietary guidelines to highly tailored meal timing, macronutrient distribution, and food choices.
In clinical practice, tools like CGM, metabolomics, and microbiome mapping are set to redefine how we manage pre-diabetes, obesity, and type 2 diabetes. This approach ensures improved glycemic control and significantly reduces long-term metabolic complications.
—
2. I follow a three-step rule: (1) simplify without diluting — convert evidence into 1–2 actionable takeaways; (2) cite one reputable source or guideline per post and avoid absolute promises; and (3) use engaging formats (short reels, infographics, myth-busting) while adding a call-to-action to consult a clinician for personalised issues. Research shows social media strongly shapes youth choices, so credibility plus clarity is essential.
Dr. Soundariya S:
Communicating science on social media requires responsibility. My approach focuses on simplifying without losing scientific integrity, citing trusted sources, and using engaging formats like infographics and myth-busting reels. Since social media heavily influences young people’s health choices, every post must balance clarity, credibility, and a reminder to seek personalised clinical guidance.
—
3. Misunderstood Myth #1 — “One probiotic or supplement fixes your microbiome.”
Reality: Recent work in precision nutrition emphasizes that microbiome’s effect on metabolism is highly individual. Diet-microbiome interactions depend on baseline gut composition, host genetics, overall diet, making one-size-fits-all probiotic/supplement claims scientifically weak.
Myth #2 — “High diversity always equals a healthy gut.”
Reality: While diversity is generally desirable, recent findings show that metabolic response depends more on functional aspects (metabolites, microbial gene expression) rather than simply taxonomy.
Myth #3 — “Dietary glycemic index/load fully predicts glycemic response.”
Reality: Emerging evidence shows that postprandial glycemic response (PPGR) is influenced not just by GI/GL, but by genetics, body composition, microbiome and meal context (timing, prior food, sleep, activity).
Dr. Soundariya S:
These myths oversimplify complex biological systems. No single probiotic can universally “fix” the gut microbiome because its metabolic influence varies by individual genetics, diet, and baseline microbial composition. Similarly, gut diversity alone doesn’t determine health—functional outputs like metabolite production matter more. Glycemic index and glycemic load also offer incomplete insight, as individual post-meal glucose responses depend on microbiome structure, lifestyle, body composition, and even sleep patterns.
—
4. A 2024 RCT showed that a personalized diet minimizing PPGR improved glycemic control better than standard low-fat diets in people with obesity and prediabetes.
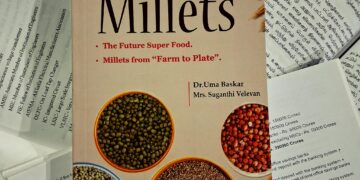
For Indian patients: Given dietary patterns (carbohydrate-heavy staples, cultural dietary habits), these advances allow for culturally adapted precision nutrition — for example: selecting local low-GI staples, optimising portion/timing based on CGM feedback, integrating microbiome-friendly foods (fibres, legumes, fermented foods), rather than prescribing Western-style diets blindly.
Dr. Soundariya S:
The 2024 RCT clearly demonstrated that personalised diets outperform standard low-fat diets in improving glycemic control. For India, where carbohydrate-rich staples dominate, this personalised approach is especially valuable. Instead of exporting Western dietary models, we can tailor nutrition using familiar, culturally acceptable local foods—optimising meal timing, portion size, and food combinations based on CGM feedback and microbiome-friendly choices.
—
5. Based on global and emerging evidence, and considering transitional dietary patterns in urban India:
Concern #1 — Increasing consumption of processed, high-GI carbohydrate foods…
Concern #2 — Irregular meal timing, late-night eating, sedentary lifestyle + poor sleep…
Concern #3 — Over-reliance on generic “diet tips” from influencers…
Recommended behavioural changes:
• Consistent meal timing with balanced, low-to-moderate GL staples
• Physical activity and adequate sleep
• Personalised nutrition assessments
• Whole-foods, fibre-rich diets; avoid restrictive fad diets
Dr. Soundariya S:
Urban India is facing a nutrition transition fueled by processed foods, disrupted routines, and social media-driven diet misinformation. High-GI foods and irregular meal timings are worsening metabolic vulnerabilities. The solution lies in returning to balanced whole-food diets, establishing consistent eating windows, improving sleep and physical activity, and promoting personalised diet planning instead of generic influencer-driven advice. These behavioural shifts significantly improve PPGR, insulin sensitivity, and long-term metabolic health.